Acoustic Neuroma
Acoustic neuromas are generally benign tumors that arise from the Schwann cells which make the myelin sheaths that insulate the nerve fibers. These tumors usually arise on either the superior or inferior vestibular nerve, so they are more properly called vestibular schwannomas. However, the term acoustic neuroma is so ingrained in common usage that it is pointless to stand on formality.
These tumors generally first come to the attention of ENT surgeons. This is because the patients will usually have hearing loss, dizziness, tinnitus, or some combination of the above as the first manifestation of the tumor. As they become larger, they will compress the cerebellum and the brainstem and eventually produce hydrocephalus. In these cases of larger tumors, headaches, gait disturbance, difficulty swallowing, or choking can also occur. As these tumors grow, hearing is usually completely lost. However, if a patient is fortunate enough to have early diagnosis, then the tumor can be removed before hearing is lost, and surgery can be performed in a technical manner to attempt to preserve hearing. With larger tumors, it is generally too late to preserve hearing. Another significant challenge of surgery on large acoustic neuromas is preservation of the facial nerve. Damage to the facial nerve will result in inability to close the eye and drooping of the face on the side of the tumor.
Treatment
Basically there are 3 strategic tracks of possible management once a diagnosis of acoustic neuroma is made. The best treatment available for these tumors involves a combined team approach of a neurosurgeon and a neuro-otologist, a subspecialty-trained ENT surgeon. This allows two experts to combine their technical expertise in both decision making and in actual care of the patients. I collaborate with my neuro-otology colleague, Dr. Sanjay Bhansali, in the treatment of these cases. These are generally long operations that take the entire day.
1. Observation with Serial Imaging
The least effective treatment is observation of the tumor without intervention. The logic that underlies this strategy is that these are generally slow-growing tumors that will take many years to reach a life-threatening size. The surgery is challenging and requires technical expertise beyond that which most general neurosurgeons receive in their training. This strategy is frequently recommended by neurosurgeons who are inexperienced in operating on these tumors. This recommendation is based on their own personal risk-benefit analysis, rather than on what may be most advantageous to the patient. Neurosurgeons who have less experience with this type of tumor believe the risk of death is low when the tumor is small, and this justifies the delay in treatment in their hands. However, the early treatment of an acoustic neuroma is not predicated solely on avoiding death from brainstem compression and hydrocephalus.
The realistic goals of early treatment by an experienced surgical team are preservation of hearing, preservation of facial nerve function, and preservation of facial sensation. Early surgical intervention when the tumor is as small as possible can be associated with high rates of functional preservation of facial nerve function and reasonable chances (in the order of 50% in some cases) of hearing preservation. While some may claim higher rates of hearing preservation, it is important to define what constitutes "hearing." The preservation of a narrow band of perceived frequencies of sound but without ability to discriminate speech, will not be of much practical value to the patient in terms of useful function on a telephone or hearing conversations in a restaurant. Another justification for observing rather than surgically removing the tumor is that hearing is generally not lost at a constant rate. Hearing is often lost suddenly such that a patient who is being observed rather than operated on will not have the luxury of noting the exact moment hearing was lost and be able to get surgery to reverse that loss. For this reason, I am not an advocate of observation in most situations unless the patient is prepared for the risk of sudden hearing loss and is comfortable with lowering his or her outcome expectations to unilateral deafness with a delayed treatment. After hearing is lost and a tumor continues to get larger, the risk of subsequent surgery to adjacent cranial nerves increases.
2. Microsurgical Treatment
This is the treatment that allows the possibility of saving hearing, saving the facial nerve, and curing the tumor with total excision. Surgery can be done using one of three different approaches to expose and gain access to the tumor: the middle fossa approach, the suboccipital or retromastoid approach, and the translabyrinthine approach. The middle fossa approach is rarely used today and is sometimes associated with injury to the temporal lobe due to retraction. The suboccipital approach is the choice made when hearing preservation is a goal because it preserves the portions of the temporal bone where the hearing and balance structures are located. It is also most suitable for larger tumors (greater than 3.5 cm) since the panoramic visibility afforded is advantageous. This approach is done by the neurosurgeon with removal of some skull behind the ear. The cerebellum is then gently retracted and under the operating microscope, the tumor is visualized. The neurosurgeon will debulk the tumor and attempt to locate the facial nerve, which is always on the deep side of the tumor between it and the brainstem. It is first located with electrical stimulation and a delicate probe. This area of tumor is carefully removed until the facial nerve is visualized. The tumor is then debulked further until only the portion extending into the internal auditory canal remains. The neuro-otologist then carefully drills the posterior wall off the internal auditory canal. Then the portion of the tumor that is in the internal auditory canal is removed and peeled away from the facial and cochlear nerves. The vestibular nerves give rise to the tumor and are therefore damaged beyond salvageability so they are removed with the tumor. Once the tumor is completely out of the internal auditory canal, and the stump of tumor at the entrance to the internal auditory canal is removed, the surgery is complete. The neuro-otologist may look down the internal auditory canal with an endoscope at this point to be sure there is no tiny retained fragment. The neurosurgeon then sews a watertight fascial graft in place to prevent spinal fluid from leaking after surgery. My practice is to reconstruct the removed portion of skull with an acrylic reconstruction. The skin is closed and the procedure completed. Throughout surgery, the electrical function of the facial nerve and the auditory nerves is monitored to minimize risk of damage.
The translabyrinthine approach may be selected for patients whose hearing has already been lost. This approach to the tumor is performed by the neuro-otologist. After several hours of drilling the petrous bone, a corridor of access is made to the tumor. This bone drilling sacrifices the petrous temporal bone which makes hearing impossible to save. After the neuro-otologist completes the bony drilling of the approach, the neurosurgeon debulks the tumor centrally and then reflects it away from the brainstem. The significant advantage to this procedure is that the facial nerve is identified early in the procedure while the temporal bone is being drilled. Its location can be used to help find the nerve on the deep side of the tumor at least at the top. This can assist in finding the nerve on the bottom side, although this surgical approach takes longer to perform. At the conclusion of this procedure, a fat graft is taken from the abdomen and laid in the bony defect created by the drilling. We place some protein glue over this to diminish the chance of a spinal fluid leak, and then the skin is closed.
Patients are generally in the hospital 3 or 4 nights depending on how they feel and on associated medical conditions.
Some different examples are shown below.
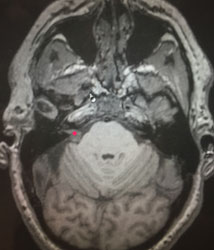
This is an example of a patient with a small acoustic neuroma that was selected for suboccipital resection for hearing preservation. This patient has partial hearing loss, tinnitus, and dizziness.
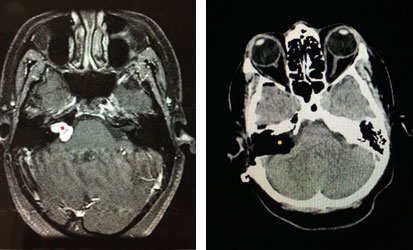
The tumor is visualized above (red dot). On the right image, the tumor has been completely resected via a translabyrinthine approach. The yellow dot highlights the black area which represents the fat graft where the bone was drilled in the approach. A complete surgical resection of the tumor was achieved, and facial nerve function was normal postoperatively.
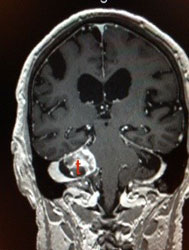
The above image shows an acoustic neuroma (t) with cystic degeneration causing gait disturbance. This is unusual since most acoustic neuromas are more solid and frequently more vascular.
3. Stereotactic Radiosurgery (SRS)
This can be done either with a gamma knife or a linear accelerator-based system. We use the latter. I do my Stereotactic Radiosurgery cases in conjunction with my Radiation Oncology colleague, Dr. Gary Stillwagon.
This treatment can be successful in long-term tumor control. The advantage to SRS is that it avoids general anesthesia and a surgical procedure. However, it is important to remember that the end point of this treatment is not typically the eradication of the tumor but control of its growth. In addition, there are risks of the tumor growing despite the treatment, in which case microsurgery will be required later. My experience is that this is associated with more difficulty in some cases owing to scarring and alteration of the tissue planes. In addition, stereotactic radiosurgery can also be associated with the same cranial nerve complications as surgery, including hearing loss, facial weakness, and facial numbness. However, this varies with various treatment planning parameters and can be optimized.

 Hablamos Español
Hablamos Español